‘Check your pressure, before it checks you’
Hyper-What?
High blood pressure, otherwise known as hypertension, is a form of cardiovascular disease (CVD). In turn, CVD is one of the most common causes of death worldwide, with as many as 1 in 3 deaths linked in some way to a diseased heart and vascular system. Hypertension has been referred to as the ‘silent killer’ because high blood pressure itself is hard to diagnose in the absence of testing. Whilst there may be downstream effects of hypertension, heart disease, half of the people with hypertension in the UK aren’t even aware of it. This equates to roughly 15% of the population blissfully ignorant of the extra strain being forced upon their cardiovascular system. The first obstacle then, is knowing your blood pressure.
How can I measure it?
When blood pressure is measured, two numbers are generated. A textbook example may be 120/80mmHg, or 120 ‘over’ 80 millimetres of mercury. The image at the top of the page demonstrates how these numbers may look on a machine. See an overview of what these numbers mean below:
1) Systolic blood pressure. This is the top number – 120 in the case above. This number refers to the pressure in the blood vessels dung systole, as blood is pumped out of the heart.
2) Diastolic blood pressure. This is the bottom number, and tends to be lower – 80 in the case above. This refers to the pressure in the blood vessels during diastole, or between beats.
Health professionals are able to take your blood pressure. Alternatively, if taking your own measurements at home with an automatic reader, there are certain precautions that must be taken to ensure repeatable and accurate readings. The American Heart Association recommends the following:
· Avoid smoking, alcohol, caffeine and exercise 30 minutes before taking the reading.
· Sit quietly for 5 minutes with the left arm comfortable supported at heart level.
· Sit with the back supported and feet flat on the floor.
· Align the cuff with the brachial artery on the upper arm.
· Rest for 1 minute between measurements. Ideally take two in the morning upon waking, and two in the evening before dinner.
Right, I have my results – are they good?
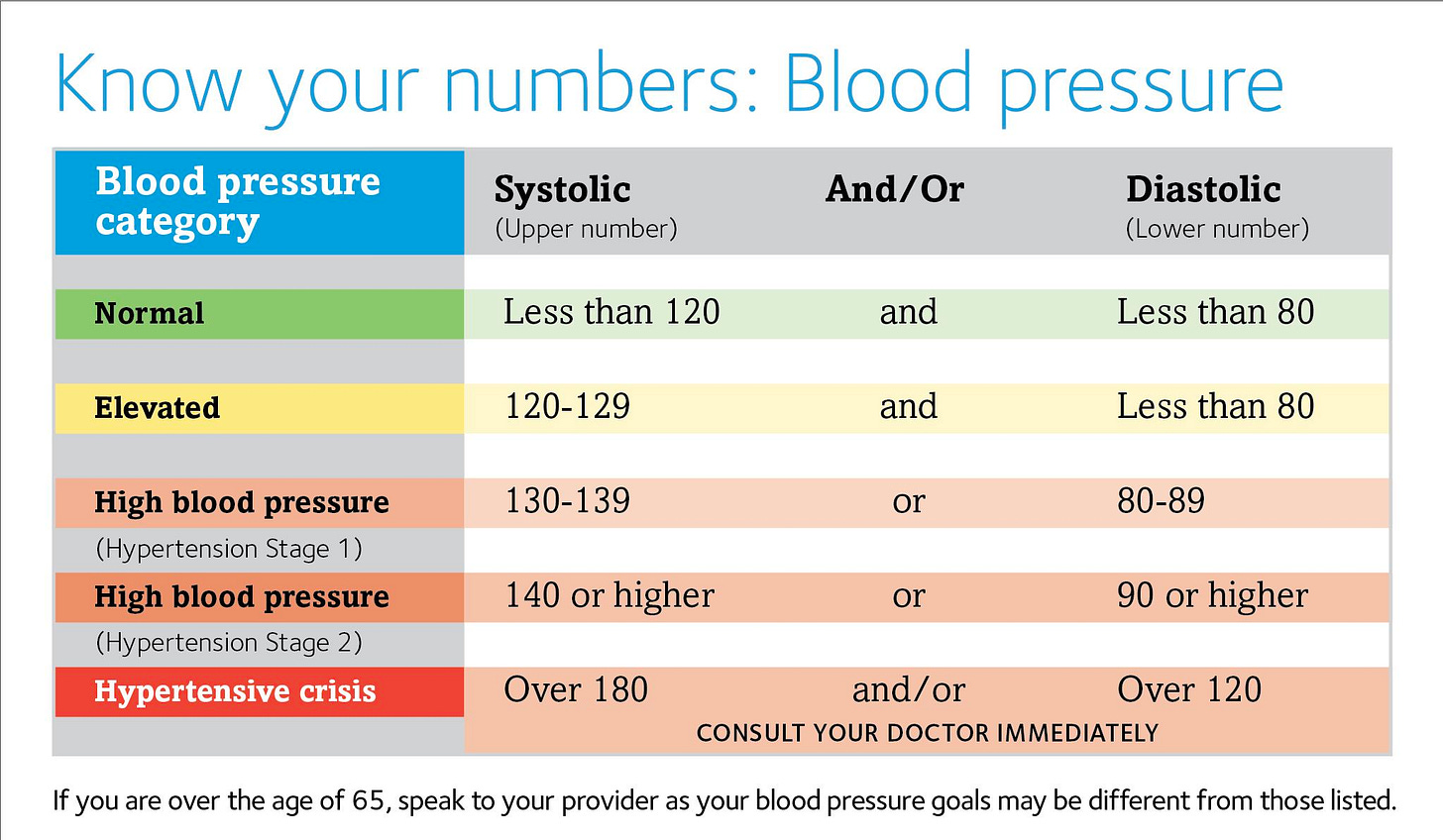
There’s a lot to unpack here, so the best bet is to use the table below, courtesy of Blood Pressure UK’s ‘Know your numbers’ drive. The table is based on AHA recommendations, but looks a bit more exciting than academic tables. Take a look.
Generally(!) speaking, aiming for 120/80mmHg is a good place to start. If blood pressure is elevated slightly (up to 130/80), then theoretically speaking, only lifestyle changes are needed to bring these numbers down. Stage 1 hypertension and above tends to require a cardiac risk assessment. These questionnaires try to estimate the risk of experiencing a cardiac event such as a heart attack in the next ten years. Depending on the results of these estimations, a balance of medication and/or lifestyle changes may be recommended.
Lifestyle Changes? Like What?
The real kicker is this: hypertension, to a reasonable extent (yes, I know, genetics…), is a lifestyle disease. If your results come back as elevated or above, lifestyle changes will be recommended regardless of the severity of the hypertension. As an exercise specialist page, I’ll go into far greater depth on the exercise recommendations later, but there are also other lifestyle changes that can be made, that I will outline below.
Diet
The DASH Diet has been shown to be an effective tool to lower blood pressure in individuals with hypertension[1]. The acronym stands for ‘Dietary Approaches to Stop Hypertension’ and puts a focus on:
- Increasing fruit and vegetable intake.
- Whole grains over refined alternatives.
- Increased intake of lean protein sources, such as poultry, fish, nuts and beans. Processed meats and red meats should be limited.
- Reduced salt/sodium intake to less than 1000mg per day.
A happy byproduct of altering diet and starting a new exercise regime could be the maintenance of, or reaching, a healthy weight. This relieves some of the stress on the cardiovascular system and also lowers blood pressure. However, this should be performed under the guidance of a professional. More on specific exercise advice to follow. Typically, a 1kg loss in weight is associated with a 1mmHg drop in blood pressure.
Cutting down on alcohol and caffeine (Here we go…)
Alcohol can increase blood pressure both acutely and chronically. As few as three drinks in one sitting can raise blood pressure and eating heart rate temporarily, whilst excessive drinking over a long period of time may lead to hypertension. General guidance advises most people to avoid binge drinking – i.e – don’t save your weekly consumption for one big night! Minimising intake to one drink each night may also be effective at lowering blood pressure, depending on previous levels of consumption.
Caffeine is a stimulant, which is ingested via tea or coffee, or even chocolate, in most people. It raises heart rate and blood pressure soon after consumption. This may not be so bad in the long run, but it will affect any at-home readings taken, if no precautions are taken.
Stress management
We live in a 100mph world. It is no longer considered ‘normal’ to take a few minutes to relax and switch off. We know that, during stressful periods, blood pressure rises. Whilst it does return to baseline once the stress is reduced, that kind of strain on the cardiovascular system is no good thing in the long run. Luckily, the tide is slowly turning, and we are starting to see a shift toward normalising these chilled moments again, as opposed to glorifying the grind. Stress and down time can take many forms. For many this may be through meditative practice, non-sleep deep rest, breathing exercises, or playing games. Others might, perhaps counterintuitively, go for a run, or take a yoga class. Perhaps more important, taking time to develop social connection and talk to friends and family is also a great way to help with stress.
Do I need to check with my doctor before I start an exercise protocol? It sounds dangerous!?
There are some generic guidelines to follow when it comes to exercise assessments in those with hypertension.
Note: Clients are considered physically active if they have already been performing 30 minutes of exercise on 3 days each week for longer than 3 months. For the following cases, it is assumed that blood pressure does not exceed 140/90mmHg on testing.
If individuals are asymptomatic and do not have any CVD, renal, or metabolic dysfunction, then they do not require any medical assessment before the completion of exercise testing.
Physically inactive clients who are asymptomatic but do have a diagnosis of CVD, renal or metabolic dysfunction should consult with a medical professional before exercise testing. If they are symptomatic, then they should also get medical clearance prior to testing.
Physically active clients who are asymptomatic but do have a diagnosis of CVD, renal or metabolic dysfunction should seek medical clearance for higher intensity exercise.
Physically active clients who are symptomatic should cease all exercise regimens and resume once medical clearance has been given.
If an individual’s blood pressure is 140-160/90-100mmHg, they should seek medical clearance prior to completing an exercise test. If blood pressure exceeds 160/100mmHg, then medical clearance is needed prior to any exercise testing and/or protocol.
Exercise testing methods - A note for the specialists

Aerobic exercise
Common sense takes charge here. For most individuals, a ramp protocol on a cycle ergometer is the most sensible option. However, treadmill may be used as an alternative where necessary. Ideally, a 12-lead ECG should be attached to allow practitioners to check for abnormal responses. If blood pressure exceeds 250/115mmHg during the test, then this should be terminated regardless of testing stage. Keep in mind that certain medications may affect the typical heart rate response to exercise.
Resistance exercise
Avoiding the Valsalva manoeuvre is recommended here. 1RM testing is recommended, but 5RM testing is also fine.
Flexibility
No extra precautions need to be taken here relative to healthy populations.
What exercise should I now perform?
Aerobic cardiorespiratory exercise
The typical guideline here is to aim for 90-150 minutes of moderate intensity aerobic exercise each week. A nice measure of intensity would be roughly 60-75% HRR, or an RPE of 12-16 on a 20-point scale. These exercise minutes should be accumulated by training on at least 2 days of the week with each session lasting at least 30 minutes. The client should also aim to be physically active at lower intensities on all days of the week if possible. This would include walking and gardening, for example.
Resistance exercise
Resistance exercise should be completing on 2-3 days each week, in line with recommendations for healthy populations. These sessions should last 20 minutes and can involve machines, free weights, resistance bands, isometric exercises[2] and callisthenics, as well as yoga or Pilates. A good template for resistance sessions would be as follows:
8-10 exercises for the major muscle groups
2-4 sets per exercise
8-12 repetitions per set
Leave at least one rest day between sessions
Flexibility
Ideally, low level flexibility training should be performed daily. A range of dynamic, static and PNF stretching is optimal, with individuals feeling the point of tightness or slight discomfort at the peak of the stretch. With static stretches, holding for up to 30 seconds at a time is recommended, with a total of 60 seconds per stretch (for example, 2x30s, or 3x20s).
Additional Notes:
· Post-exercise hypotension is a known phenomenon which results in lower blood pressure on exercise days relative to rest days. This has resulted in recommendations for hypertensive individuals to exercise on most, if not all, days.
· There is promising research to show that neuromotor exercises like Tai-Chi can be very effective for lowering blood pressure in hypertensive individuals. If this is a more gentle way of introducing movement, and creating habits, then by all means, try it!
So…what next?
As you can probably tell here, exercise lifestyle modification and medication are the three keys to lowering blood pressure. Provided that you stick to the guidelines above, more exercise is better than less, and may result in better reductions in blood pressure. Ultimately, the real challenge lies in finding a regimen that the individual in question can stick to. It is better to do something every day than it is to perform a big effort once a week. That is where our expertise comes in handy, and, ultimately, that is what we are paid to create.
[1] Siervo, M. et al. (2015) ‘Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis’, British Journal of Nutrition, 113(1), pp. 1–15. doi:10.1017/S0007114514003341.
[2] Edwards JJ, Deenmamode AHP, Griffiths M, et al. Exercise training and resting blood pressure: a large-scale pairwise and network meta-analysis of randomised controlled trials. British Journal of Sports Medicine 2023;57:1317-1326.